
Building climate-resilient rural communities
British Columbia
CLIMATE CHANGE IN THE GLOBAL CONTEXT
Scientific evidence shows that our climate is warming. Global average surface temperatures have risen by 0.9°C in the last 100 years, which can be attributed to increases in human driven greenhouse gas emissions (for example, by burning fossil fuels). This rise in temperature has been accompanied by observed increases in extreme weather events, sea level rise, glacier melt, ocean acidification, and declines in arctic sea ice. Climate change is also expected to increase existing global socio-economic inequities.
CLIMATE CHANGE IN THE CANADIAN CONTEXT
Changes in Canada’s climate will have consequences to the health, wellbeing, and livelihoods of Canadians, especially the most vulnerable population, and the natural ecosystems they depend on for survival. Both COVID-19 and climate change pose implications on public health and economic stability in Canada. Canada’s climate has warmed and continues to increase in mean temperature rise. Evidence shows that observed warming in Canada is likely due to the influence of human activities like build-up of greenhouse gases. Regional differences and similarities in climate change hazards and its effects in Canada can be found here .
CLIMATE CHANGE IN BRITISH COLUMBIA
In the past century, the average temperature of B.C. rose by 1.4°C. In particular, Northern B.C. has shown a 2°C increase, that is twice the global average. By 2080, BC’s temperature is projected to further increase for up to 4.5°C, more than three times of what was seen in the past century. Climate impacts such as water shortage, drought, wildfires, and floods are seen in different parts of the province. Rural communities are more vulnerable due to their limited resources and increased dependency on the environment. Risk assessment based on geographic location, population demographic, and availability of infrastructures will be the first step in mitigating and adapting to the ecosystem disruption we see today, and is subject to progress in the future.
To understand and respond to climate change impacts in B.C., it is essential to identify population groups most vulnerable to these impacts to tailor relevant mitigation/adaptation measures.
POPULATION VULNERABLE TO CLIMATE CHANGE IN B.C.
- Indigenous peoples
- Rural and remote communities
- Population over 65 years of age

Click ">>" to the top left corner of the map for more details.
RURAL, REMOTE & INDIGENOUS PEOPLES:
Many rural & remote communities in B.C. have close relationships with and dependence on the natural environment which may be disrupted by climate change. Though many Indigenous communities demonstrate immense land-based knowledge and capacity to adapt to ecosystem disruption, Indigenous populations face a high burden of poor health due to the historical and on-going impacts of colonialism and socio-economic inequities, which may impede their ability to adapt to climate change.
ELDERLY POPULATION OVER 65 YEARS OF AGE:
Age is an important risk factor for almost all climate change-related health outcomes. Underlying acute and chronic diseases can exacerbate with higher age groups.
Heatwaves and increased humidity are associated with higher all-cause mortality rates in individuals of 65+ years. Respiratory, cardiovascular, and nervous system-related deaths were especially prominent. The ageing population has increased in rural areas more than urban areas with mental health outcomes much worse in rural areas.
In addition to the population disproportionately impacted by climate change, we must also identify natural hazards in rural areas.
Watch this video by B.C. Public Service to learn about the importance of disaster studies in disaster preparedness and management in B.C.
Source: Government of British Columbia. B.C. Public Service. Available from: https://www.youtube.com/watch?v=me3o4qHh51g&ab_channel=BCPublicService, 2018
Lets look at some of the most pressing climate hazards in B.C.!
CLIMATE HAZARDS IN B.C.
Many of these climate hazards may lead to negative health outcomes.
Lets explore the connection between increasing health outcomes, as a result of climate change hazards!
CLIMATE CHANGE RELATED HEALTH IMPACTS IN B.C.
Climate change hazards impacts health determinants and health outcomes. Population and community health is influenced by health determinants that includes socio-economic, cultural and environmental factors. The infographic illustrates that climate hazards impacts health determinants which in turn influence physical and mental health outcomes.
Learn more about climate related health outcomes here.
INFECTIOUS DISEASE
The emergence and severity of infectious disease is highly dependent on the natural environment. Though the relationship between climate change and infectious disease spread is complicated and still poorly understood, climate change will alter the geographic and seasonal distribution of these diseases.
MENTAL HEALTH
The unprecedented progression of ecosystem disruption, increased rates of extreme events, and subsequent health outcomes can have significant impacts on our personal lives. This can be in the form of general despair, financial losses, disruption of daily tasks, and loss of social connections. Such dramatic changes tend to produce increased incidence of depression, anxiety, posttraumatic stress disorder (PTSD), and other manifestations of poor mental health.
RESPIRATORY HEALTH
Most of our everyday practices, from transportation, burning of fossil fuels, to waste disposal contribute to increasing levels of particulate matter (PM) and carcinogens such as black carbons. Accumulated exposure to such air pollution increases our lifetime risk of developing lung cancer, asthma, chronic obstructive pulmonary disease (COPD), and allergies. Wildfires, in addition to longer-term air pollution, can produce immediate spikes in acute respiratory damages. This includes respiratory tract burns, difficulty breathing, bronchitis, and exacerbation of preexisting respiratory diseases.
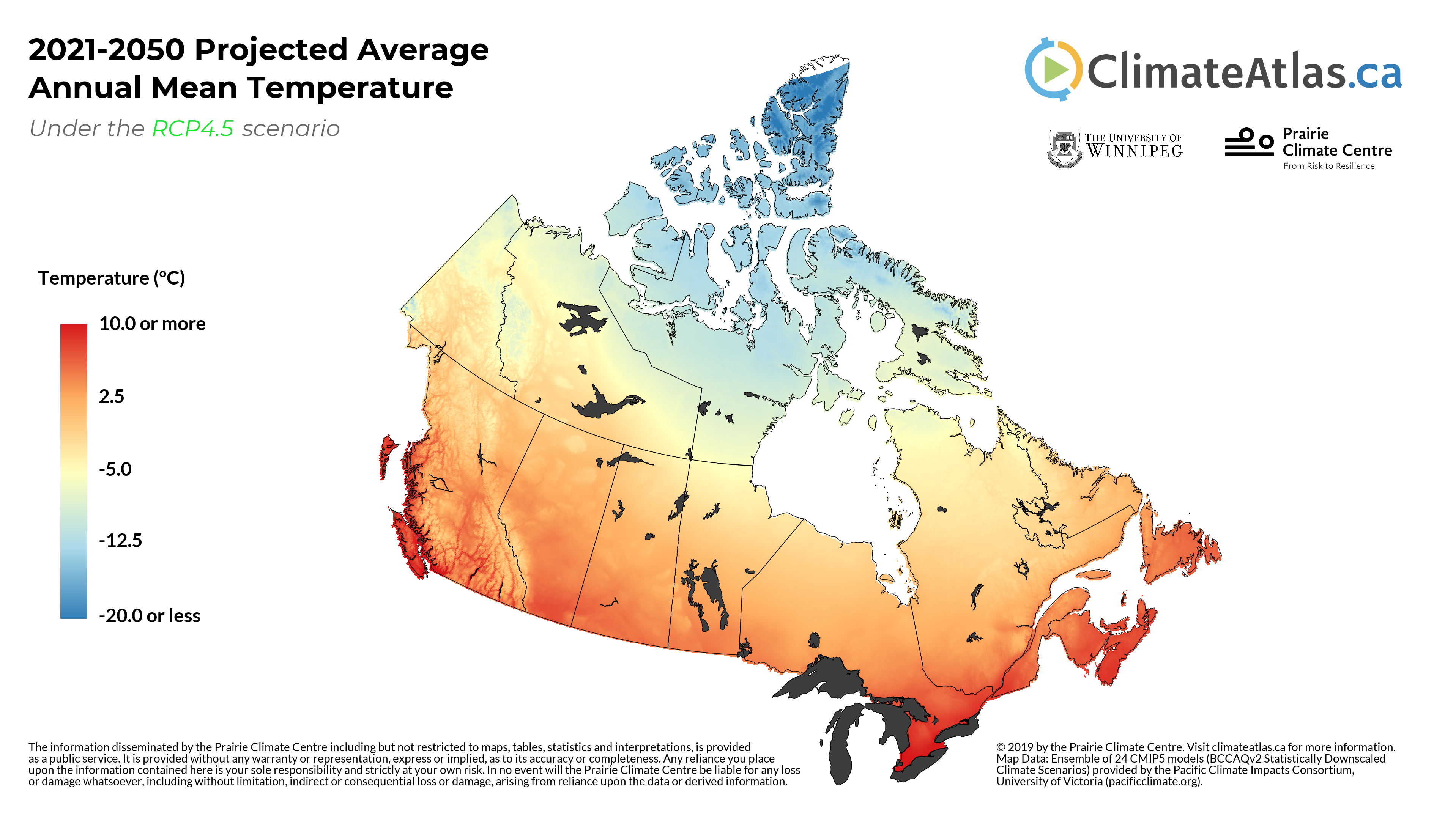
TEMPERATURE - RELATED MORBIDITY & MORTALITY
Increased temperatures pose significant health risks. A growing body of evidence suggests that there will be large increases in average annual temperatures in British Columbia over the next 30 years, raising concerns for heat-related morbidity and mortality.
Observed increases in temperature and heat-related morbidity and mortality in British Columbia have been the greatest in the Interior. Elderly populations and those who work in outdoor environments are at the greatest risk for heat-related morbidity and mortality.
FOOD & WATER SAFETY
Climate hazards, such as increases in precipitation and temperature, may compromise food and water quality, as well as increase the incidence and severity of food- and water-borne diseases.
Rural and coastal communities are at high risk as these communities are dependent on small, private systems, and communities whose water sources are influenced by the Northern Pacific ocean and have been identified as vulnerable to climate-driven changes to water-borne diseases.
Forecasting food-borne disease risks is more challenging as relationships between food, food-borne illness, and changes in temperature and climate are complex and unpredictable. Increasing research to improve predictive capacity and creating adaptable food systems may mitigate some of the negative impacts.
To learn more about Climate hazards and the associated health impacts
As climatic conditions continue to alter, natural hazards continue to increase in frequency and intensity causing negative health impacts. It is essential to integrate climate change adaptation into communities, especially those at-risk to reduce morbidity and mortality from natural disasters.
Source: Stacy Barter and Kerri Klein. Health Authority Perceptions and Capacity for Action: Health Impacts of Climate Change in BC. BC Healthy Communities Society, 2013.
Lets look at some climate Adaptation and resilience action in rural communities of B.C.
CURRENT CLIMATE CHANGE ADAPTATION PROGRAMS IN RURAL B.C.
Click on the location icons!
Lets look at some climate change adaptation strategies implemented to bolster community health!

Kanaka bar Climate adaptation strategy
Kanaka bar Climate adaptation strategy. Click to expand.

Cariboo climate adaptation
Cariboo climate adaptation. Click to expand.
Communities: Main centers include Williams Lake, Quesnel, District of 100 Mile House. The remainder of the population lives in rural areas of in 15 Secwepemc, Tsilhqot’in, and Carrier communities belonging to those language groups.

Nisga’a adaptation program
Nisga’a adaptation program. Click to expand.
Community: Lax Bilak
Elkford is a rural community surrounded by sub-alpine forests, meadows, and lakes of the Rocky Mountains, home to a beautifully diverse ecosystem. With a total population of 2,499 (2016 Census), more than half (59%) are between ages 25-64 [1] .
With the rising climate change risks and impacts, Elkford is one of many rural communities in BC that are facing dramatic disruptions in their ecosystem. Elkford has already experienced up to 2°C increase in temperature and is projected to warm an additional 3°C by 2050. Subsequent droughts are increasing Elkford’s risk of wildfires and pine beetle infestations in their forests. Destruction of trees in turn makes the community susceptible to flooding during winter rainfalls [ 2 , 3 ]. Such environmental disruptions can lead to severe health risks and outcomes. These include: contaminated water supplies and spread of water-borne infectious diseases; respiratory illness from air pollution and forest fires; heat stroke and dehydration; and mental health disruption from loss of homes, jobs, and loved ones[ 4 , 5 ].
Adaptive action plans are required to protect the community and wildlife that depend on Elkford’s natural habitat. This virtual reality experience will help us understand how climate change impacts BC’s rural and remote communities, and how to support in building resiliency for its people and the environment.
Issue:
Large wildfires in the greater Elk Valley region occurred in 1904 and 1908, the years when the town of Fernie was destroyed by wildfires. Wildfires may have also occurred in the Fording Valley in the 1960’s.
"In 2003, the Lamb Creek and Plumbob fires burned significant areas in the East Kootenay"
These areas were identified as high to extreme fire risk:
- Northwest of North Elkford
- Northeast of North Elkford
- East of South Elkford
Response:
The District of Elkford developed a Wildfire Management Strategy which includes a Fuel hazard ranking and wildfire risk analysis based on an assessment of the forest fuel types and historical weather patterns in the region. See here for specific recommendations for wildfire mitigation.
The District of Elkford also has integrated wildfire planning into their Official Community Plan (OCP) which includes considering fire prevention and layout of any buildings in high risk areas and capacity to accommodate emergency vehicles in roadways and turnabouts and providing them the right of way in road access in incomplete.
Issue:
Increased frequency and severity of floods has had major negative impacts in Elkford (floods, mudslides, landslides).
Response:
In response to flooding, Elkford began an initial study in 2009 and after significant flooding in 2013 caused serious damage they were able to secure provincial funding to conduct repairs along Boivin Creek.
In 2008, Elkford, a local Adaptation Strategy that assesses the risks posed by climate change and identifies corresponding adaptation actions.
The Adaptation Strategy was developed concurrently with a revision to Elkford’s Official Community Plan (OCP), allowing the two to be fully integrated, a first in British Columbia. A Community Advisory Committee provided guidance and ensured community priorities were reflected throughout the process.
Click here to learn more
PROPOSED CLIMATE ADAPTATION STRATEGIES FOR RURAL HEALTH SERVICES
Citizen/community voice:
Community members are one of the most important partners as they hold local knowledge, experience, and connection to the environment that acts as an impetus for effective climate change adaptation. Community engagement is particularly important for health services, because health heavily depends on individual lifestyle and choices. Health literacy and awareness of resources are fostered through direct participation in health planning, contributing to improved population health.
Indigenous ways of knowing:
Health services must incorporate Indigenous knowledge and traditions as they are deeply connected to our environment, and can provide important perspectives to climate adaptation. They are one of the first to face direct consequences of climate change due to their close relationship with the environment and its resources. Enhancing the adaptive capacity of Indigenous peoples will only be successful if integrated alongside the other adaptation strategies.
Emergency preparedness:
Building climate resilient rural communities starts with conducting vulnerable risk assessments and target response strategies for climate-induced emergencies (ex. Forest fires, heat stress, floods, infectious disease outbreak etc). Emergency preparedness adaptation for rural health services may include maximizing local services capacity and volunteerism, and adequate infrastructural capacity to minimize adverse health outcomes from these events.
Telehealth:
Geographic isolation between rural communities and from the nearest referral centres make it harder for residents to seek care. Telehealth increases accessibility to various types of health services without additional economic, social, and psychological burden on patients and families while also reducing the carbon footprint generated by the need for medical transport and accommodation.
Generalism & Enhanced skills/team-based care:
Adverse health outcomes from climate change are complex, because of the various environmental consequences of climate change such as natural disasters, infectious diseases and temperature changes. To make matters more complex, outcomes will depend on numerous factors such as age, existing illnesses, geographic location, local ecosystem, and much more. Generalism is particularly important for rural and remote communities because of limited resources such as required infrastructure for specialized care, attributed partly to the size of the population. Generalists with enhanced skills allow for availability of local health services and contribute to keeping healthcare closer to home.
Research Symposium!
Please join us on Nov 30th - Dec 1st for our research symposium on climate change and rural health services adaptation. We look forward to continuing our conversation on climate adaptation and rural health services there.
If you are working on climate change projects, or would like to share stories or experiences of climate change impacts in your communities, please reach us at
We will share your experience on this storyboard on an ongoing basis.
We are open to all feedback and recommendations for this storyboard!